Suicide Prevention: Taking Care of Others and Taking Care of You
According to a recent study published by the Center for Disease Control, reported suicidal ideation among American adults had doubled by June 2020 in comparison to previous years. According to the American Foundation for Suicide Prevention:
- Suicide is the 12th leading cause of death in the US.
- In 2020, there were an estimated 1.2 million suicide attempts.
- On average, there are 130 suicides per day.
- The rate of suicide is highest in middle-aged white men.
[1] Czeisler MÉ , Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1049–1057. DOI: http://dx.doi.org/10.15585/mmwr.mm6932a1.
TAKING CARE OF OTHERS WHEN THERE IS CONCERN OF SUICIDAL IDEATION OR ACTION
When the topic of suicide comes up, it is often hard to know how to react. Knowing what to do or say during such a situation does not come naturally to many. Being informed and knowing where to find help and support for the individual in need or yourself is crucial to preventing a suicide attempt or completion.
SIGNS OF SUICIDAL IDEATION
Read More...
- Threatening to hurt or kill themselves
- Actively seeking ways to kill themselves
- Talking, writing, or posting about death, dying, or suicide
- Hopelessness
- Rage, anger, seeking revenge
- Reckless or risky behavior
- Feeling trapped (as if there is no way out)
- Increasing drug/alcohol use
- Withdrawing from friends, family, or society
- Anxiety, agitation, sleep disruptions
- Dramatic changes in mood
- No sense of purpose in life
RISK FACTORS OF SUICIDE
Suicide happens across all genders, ages, ethnicities, socioeconomic status, and lifestyles, however, the following are factors that are most likely to lead to the completion of a suicide attempt, according to the National Institute of Mental Health:
Read More...
- Depression, other mental disorders, or substance abuse disorder
- Certain medical conditions
- Chronic pain
- A prior suicide attempt
- Family history of a mental disorder or substance abuse
- Family history of suicide
- Family violence, including physical or sexual abuse
- Having guns or other firearms in the home
- Having recently been released from prison or jail
- Being exposed to others' suicidal behavior, such as that of family members, peers, or celebrities
DOMESTIC VIOLENCE & SUICIDALITY
One key risk factors of suicidality to recognize is the presence of family and/or domestic violence. Survivors of intimate partner violence are twice as likely to attempt suicide multiple time, according to the American Psychology Association.
Read More...
Domestic abuse can look like…
- Overprotectiveness, jealousy, accusations of disloyalty
- Controlling finances, denying access to finances or other assets
- Controlling where the partner goes, who they see, what they do
- Embarrassing a partner using bad names or put downs
- "Punishing” a partner with guilt or arguments after they've spent time with family or friends, which causes them to withdrawal from important relationships
- Looking at a partner or acting in ways that scare them
- Threatening to commit suicide or to kill their partner
- Acting like abuse is not a big deal, denying abuse, or blaming their partner for the abuse
- Hitting, slapping, punching, kicking, shoving, biting, strangling
- Threats of violence against partner, children, pets, or other family members or friends
- Intimidating their partner with guns, knives, or other potential weapons
- Driving recklessly or dangerously when their partner is in the car with them
- Destruction of property, abuse of animals
- Forcing their partner to have sex or perform sexual acts against their will
If you believe that you or someone you know is experiencing domestic abuse, please call Family Crisis Centers Crisis Line at 800-382-5603 or visit https://www.familycrisiscenters.org for more information.
DO's AND DON'T's OF SUICIDE PREVENTION
The National Suicide Prevention Lifeline advises the following:
Read More...
- Be direct. Talk openly and matter-of-factly about suicide.
- Be willing to listen. Allow expressions of feelings. Accept the feelings.
- Be non-judgmental. Don't debate whether suicide is right or wrong, or whether feelings are good or bad. Don't lecture on the value of life.
- Get involved. Become available. Show interest and support.
- Don't dare them to do it.
- Don't act shocked. This will put distance between you.
- Don't be sworn to secrecy. Seek support.
- Offer hope that alternatives are available but do not offer glib reassurance.
- Take action. Remove means, like weapons or pills.
- Get help from people or agencies specializing in crisis intervention and suicide prevention.
HOW TO HELP SOMEONE STRUGGLING
Seasons Center recommends following #BeThe1's 5-Step Action Plan for helping someone who is experiencing suicidal ideation. If someone appears to be in imminent danger or risk of harm, please do not hesitate to call 911. Please visit https://www.bethe1to.com/bethe1to-steps-evidence for further details on this action plan.
Read More...
- Ask
- "Asking the question "Are you thinking about suicide?” communicates that you're open to speaking about suicide in a non-judgmental and supportive way.”
- Be there
- "This could mean being physically present for someone, speaking with them on the phone when you can, or any other way that shows support for the person at risk. An important aspect of this step is to make sure you follow through with the ways in which you say you'll be able to support the person.”
- Keep them safe
- "After the "Ask” step, and you've determined suicide is indeed being talked about, it's important to find out a few things to establish immediate safety” including have they attempted suicide previously, do they know how they would attempt suicide, do they have a detailed plan, etc.
- Help them connect
- "Helping someone with thoughts of suicide connect with ongoing supports (like the Lifeline, 800-273-8255) can help them establish a safety net for those moments they find themselves in a crisis” by going through their options such as providing them with ideas for reaching out for professional mental health help or inquiring about what has helped them in the past. Additionally, creating a safety plan could also be helpful (see the SAFETY PLANNING dropdown menu for more information)
- Follow up
- "After your initial contact with a person experiencing thoughts of suicide, and after you've connected them with the immediate support systems they need, make sure to follow-up with them to see how they're doing. Leave a message, send a text, or give them a call.”
SAFETY PLANNING
A safety plan is physical document that is created by and for the individual experiencing suicidal ideation. In times of distress, this document should ideally help guide them away from a suicidal crisis. According to the Centre for Suicide Prevention, safety plans include:
Read More...
- their personal warning signs,
- coping strategies that have worked for them in the past, and/or strategies they think may work in the future,
- people who are sources of support in their lives (friends, family, professionals, crisis supports),
- how means of suicide can be removed from their environment, and
- their personal reasons for living, or what has helped them stay alive.
Additionally, #BeThe1 recommends the mobile app My3 for creating an easy and straight forward digital safety plan.
MORE RESOURCES AND LINKS
Read More...
TAKING CARE OF YOU: TRAUMA AND ITS IMPACTS
After having helped another through a suicidal or general mental health crisis, it is important to consider the emotional impacts such interventions have on us as the support person. Prioritizing taking care of yourself can heal emotional scars as well as allow you to be prepared to help someone else in need, if another situation should arise.
DEFINITIONS: TRAUMA AND BURNOUT
Read More...
Trauma is defined as "an emotional response to a terrible event or repeated occurrence like an accident, abuse, or natural disaster.”
Secondary trauma occurs through "indirect exposure to trauma through a firsthand account or narrative of a traumatic event.”
As a result, the event, series of events, set of circumstances, or secondary trauma has negative lasting effects on the individual's daily functioning and mental, physical, social, emotional, or spiritual well-being.
NOTE: Trauma is defined by the individual who experienced the trauma. What may be traumatic for someone else, may not be traumatic for you and vice versa.
Both trauma and secondary trauma can lead to burnout, which is defined as "a long-term stress reaction marked by emotional exhaustion, depersonalization, and a lack of sense of personal accomplishment.”
Definitions from the Psychiatric Times, The American Psychological Association, SAMHSA-HRSA Center for Integrated Health Solutions, and The Agency for Healthcare Research and Quality.
SIGNS OF TRAUMA
According to The Mayo Clinic, trauma can show up in many forms:
Read More...
- Intrusive memories
- Recurrent, unwanted distressing memories
- Reliving of traumatic events
- Upsetting dreams/nightmares
- Severe emotional distress/physical reactions when something reminds you of traumatic events
- Avoidance
- Trying to avoiding thinking/talking about traumatic events and avoiding places, activities, or people that remind you of the traumatic events
- Negative changes in thinking and mood
- Negative thoughts about self, world, and others; hopelessness toward future
- Memory problems
- Difficulty maintaining close relationships
- Feeling detached from family/friends
- Lack of interest in activities you once enjoyed
- Difficulty experiencing positive emotions
- Feeling emotionally numb
- Changes in physical and emotional reactions
- Being easily startled or frightened
- Always being on guard for danger
- Self-destructive behavior (drinking too much, driving too fast, experimentation with substances)
- Trouble sleeping; trouble concentrating
- Irritability, angry outbursts, or aggressive behavior
- Overwhelming guilt/shame
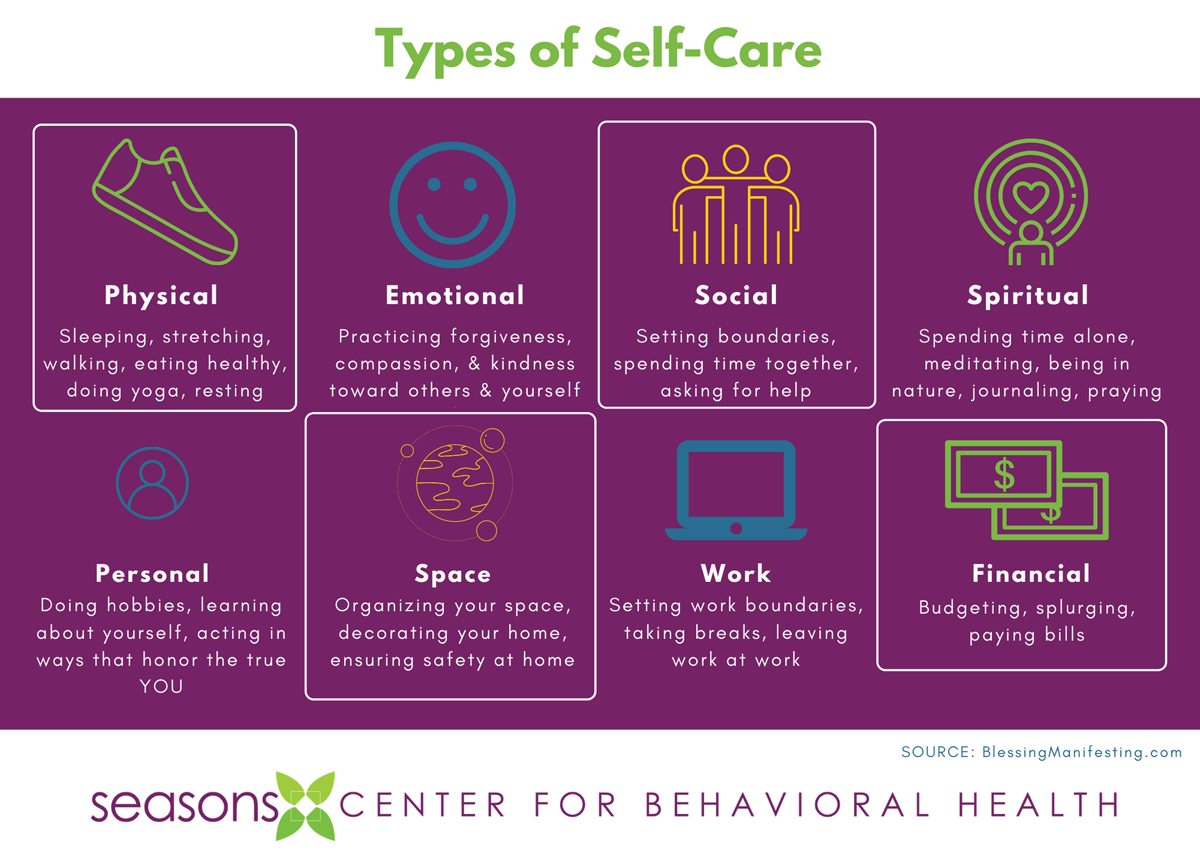
SELF-CARE
Self-care is the "practice of taking action to preserve or improve one's own health” including one's mental, physical, social, emotional, or spiritual health. Often when talking about "self-care", we hear the expression "you can't pour from an empty cup.” Self-care is any activity that you take part in that "fills your cup." It is anything that brings you joy, relaxation, and time for you to detach from your life stressors.
Read More...
Why should I practice self-care?
- Prevents burnout and exhaustion
- Build resilience (i.e., your ability to "bounce back" from stress, trauma, or burnout)
- Helps improve sleep
- Improves focus
- Strengthens your relationships (by taking care of YOU, you are more equipped to care for others)
- Generally increases feelings of happiness, joy, and gratitude
Tips for Practice
- Make sleep part of your self-care routine.
- Take care of yourself by eating healthy and exercising daily.
- Learn to say no to others, and yes to self-care.
- Take a self-care break by getting outside.
- Let a pet help you with your self-care.
- Take care of yourself by getting organized.
- Read up on self-care.
- Schedule time for self-care.
What counts as self-care?
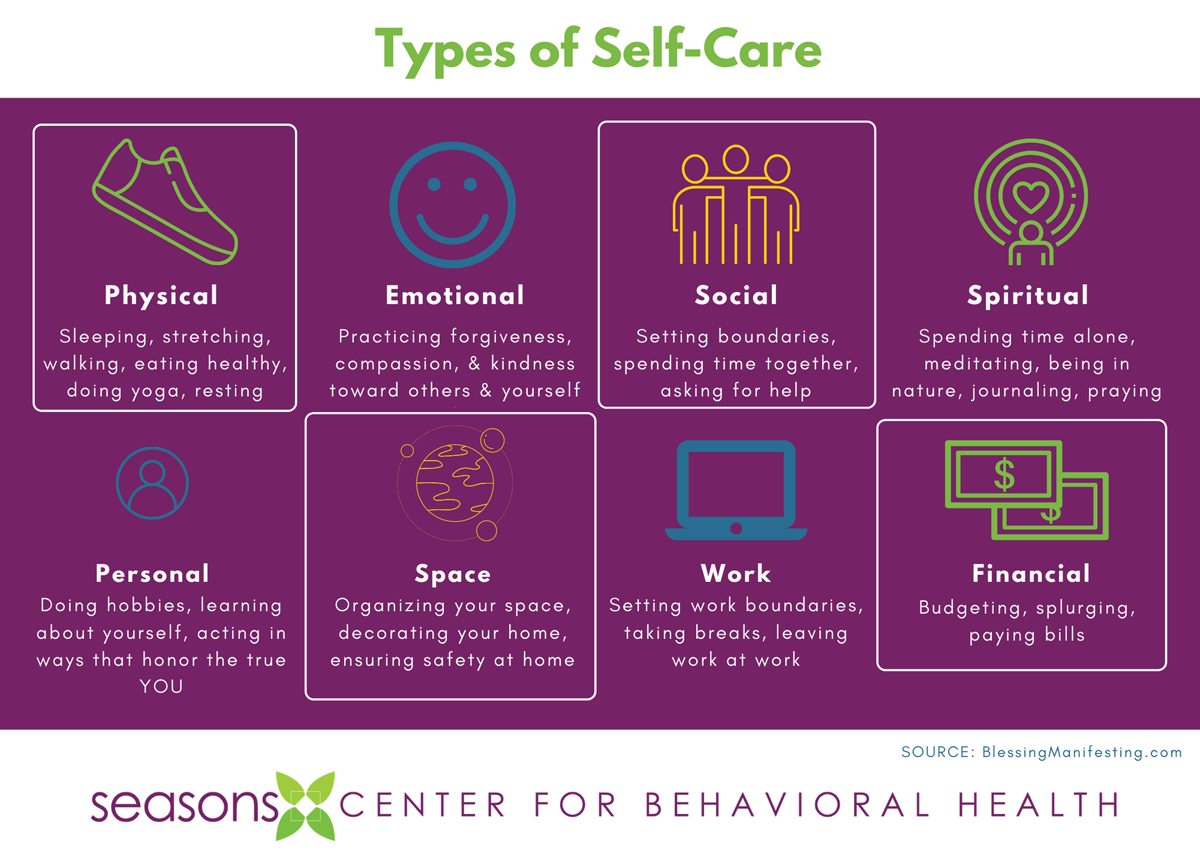
Information gathered from FindYourWords.org, Psychology Today, and BlessingManifesting.com.
SEEKING HELP
According to the Association for Behavioral and Cognitive Therapies, you should consider seeking professional help if you:
Read More...
- Are feeling unhappy or generally dissatisfied with life
- Feel you could use support when coping with stressful life events or trauma
- Are having troubles completing normal daily tasks
- Feel you are spending less time with family, friends, or children and/or feel unengaged when you do so
- Have been late to work, missing work, or having issues completing work tasks more frequently
- Have been isolating or withdrawing from important social relationships with family or friends
- Feel like being with family and friends is draining.
- Have noticed negative changes in your body or mind including (but not limited to) change in appetite, energy, or sleep, heightened anxiety, excessive worry, etc.
- Have lost interest in activities you used to enjoy
Please visit https://www.abct.org/Information/?m=mInformation&fa=DecidingWhenToSeek for specific questions to ask yourself when wondering if you should seek mental health treatment.
MORE RESOURCES AND LINKS
Read More...
HELPLINES
- 988 Suicide & Crisis Lifeline
- Seasons Center's 24/7 Crisis Line (844)-345-4569
- Post-Trauma Stress Disorder Hotline (844)-289-0879
- National Alliance on Mental Illness Helpline (800)-950-NAMI (6264) or text NAMI to 741-741
- Your Life Iowa Line (855)-581-8111
- National Sexual Assault Hotline (800)-656-HOPE (4673)
- Veterans Crisis Line (800)-273-8255 (press 1) or text 838255
If you or someone you know is in immediate danger, call 911.